ICBP Phase 1 Research
ICBP Phase 1 showcase report
Read about new research findings and impacts of the ICBP
ICBP findings from Phase 1 showed the following:
-
Cancer survival improved between 1995 – 2007 for all jurisdictions, but differences still existed
-
Survival during this period was higher in Australia, Canada and Sweden, intermediate in Norway and lower in Denmark and the UK (England, Northern Ireland and Wales)
-
A new method to compare different countries’ cancer data was first used for this study and showed significant differences in stage distribution and stage-specific survival between age groups
-
More missing stage information was identified in the older age groups
-
The analysis highlighted the importance of having consistent and high-quality data on stage at diagnosis to enable further insights to be generated
-
A large survey study identified reasons why the public might not visit their doctor if they had a symptom of cancer across all jurisdictions
-
The referral of patients from primary care doctors to diagnostic tests might differ across the jurisdictions, which could impact survival outcomes
International cancer survival benchmark (1995-2007)
|
An analysis of 2.4 million cancer patient records showed that overall survival rates improved in all jurisdictions between 1995 and 2007. Survival was higher in Australia, Canada, and Sweden, intermediate in Norway and lower in Denmark and the UK (England, Northern Ireland and Wales). The 5-year survival estimates for ICBP cancer types from 1995-2007 is demonstrated on the graphs [1] |
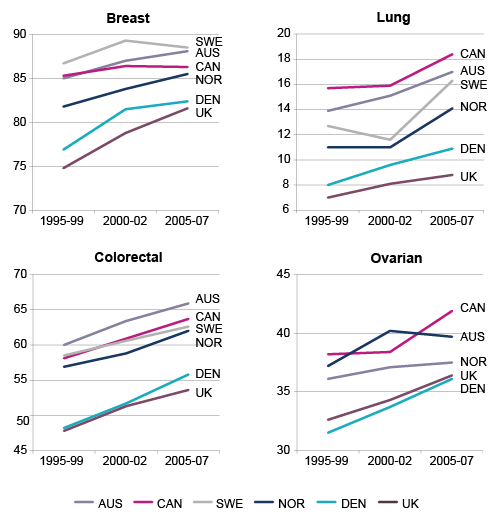 |
The survival ‘gap’ between the countries with the highest and the lowest survival estimates remained largely unchanged- except for breast cancer, where the UK saw improvements and a narrowing of the gap.
This study saw a new and innovative way to compare different countries’ cancer data. The data comparison showed significant differences in the correlation between cancer stage at diagnosis and survival between age groups. Missing stage information was also highlighted as an issue for older groups. The analysis demonstrated the importance of having consistent and high-quality data on stage at diagnosis to enable further insights to be generated.
Cancer survival benchmark using population-based registry data (2011)
Awareness, attitudes and beliefs about cancer
This module investigated the general public’s awareness and attitudes towards cancer to see if cultural differences could help explain variation in survival between jurisdictions. It was acknowledged that individuals with low awareness of cancer symptoms or negative beliefs about cancer outcomes may delay going to the doctor when they have symptoms.
The study found similar levels of cancer symptom awareness and generally positive beliefs about cancer across all jurisdictions. There was low awareness across all jurisdictions that age is a risk factor for cancer. Respondents in the UK reported the highest number of barriers to seeing their primary care physician (PCP). The findings from this study continue to demonstrate the need for public awareness campaigns to encourage presentation to PCP’s, particularly for older people at risk.
Awareness, attitudes and beliefs about cancer across ICBP jurisdictions (2013)(link is external)
The role of primary care physicians in diagnosing cancer
This study explored differences in how primary care physicians (PCPs) manage patients with cancer symptoms. PCPs completed a survey that included questions about the environment they work in and the course of action they may take to patients and different types of symptoms.
PCPs in England, Northern Ireland and Wales consistently reported a lower readiness to refer or investigate patients with potential cancer symptoms than other jurisdictions. The results suggest that differences in PCPs’ access to diagnostic tests and how they interact with different services within the local health system may be having an impact on how they are able to manage patients.
A health systems ‘mapping’ exercise confirmed differences between ICBP jurisdictions that would need further investigation. Examples include the nature of a patient’s contribution to health care costs and the ease with which patients can move freely between primary care providers. Such factors may impact on patient or doctor behaviour and could contribute to differences in cancer outcomes.
How might healthcare systems influence the speed of cancer diagnosis? (2014)(link is external)
Measuring time intervals and pathways from symptoms to diagnosis and treatment
This module compared the routes for diagnosis and time intervals from patients first noticing a symptom to starting treatment across the ICBP countries. Surveys were conducted amongst breast, colorectal, lung and ovarian cancer patients, their primary care practitioners (PCPs) and their cancer treatment specialists (CTSs).
There was marked variation between ICBP jurisdictions in the following time intervals:
- The point when the patient noticed their symptoms, until they presented within their healthcare system
- The time taken from when the patient presented at their healthcare system to their diagnosis of cancer
- The time taken from diagnosis until treatment
These findings warrant further investigation of how the different ICBP health systems organise their services, what is available for PCPs in diagnostic and referral services, and what services are offered to patients.
Another study within this module also found variation in time intervals for lung cancer patients. The study also found the main route for patients to be diagnosed with lung cancer was after them presenting to their PCP. The most common symptoms reported to PCPs was persistent cough and breathlessness, however it was found PCPs were reporting fewer symptoms than patients were, particularly weight loss and fatigue.
Diagnostic routes and time intervals for patients with colorectal cancer(link is external)
Impact of differences in cancer registry processes
High quality, population-based registry data plays a central role in the way we try to understand how to improve outcomes for people affected by cancer. In order for us to make international survival comparisons it is important to ensure we have reliable and comparable cancer registry data from our participating jurisdictions. This module of research assessed and estimated the combined effects of differences in cancer registration practices on 1-year survival on an international scale.
It was found that cancer registries use different rules to define the date of a cancer diagnosis and differ in how they handle death certificates and multiple primary tumour cases. The largest difference found in 1-year survival between the original Phase 1 ICBP benchmark and the survival estimates after taking into consideration the registry practice differences was 7.3% for lung (in Norway and Ontario), 3.4% for colorectal (in Sweden), 2.6% for ovarian (in Norway) and 1.3% for breast (in Ontario).
These findings do not fully explain the survival gap that exists between the UK (England, Wales, Northern Ireland) and those jurisdictions with higher 1-year survival but it could mean that some of the jurisdictions originally reported to have the best survival outcomes (Norway, Sweden, Ontario) may not be performing as well comparatively as originally thought.
ICBP Phase 2 research involves a systematic approach to understand how registry processes, clinical practice, ad variation in stage at diagnosis impact short-and long- term survival.
Additional Phase 1 Publications
Comparability of ICBP stage data (2012)
Ovarian cancer survival and stage at diagnosis (2012)
The ICBP: An international collaboration to inform policy (2013)
Breast cancer survival and stage at diagnosis (2013)
Colorectal cancer survival and stage at diagnosis (2013)
ICBP Blogs: Phase 1 Research
See also
References
[1] Coleman MP, Forman D, Bryant H, et al. Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet 2011; 377(9760):127-138.
Join us on social media
Join the conversation and follow the ICBP on LinkedIn, X (formerly Twitter) and YouTube to stay informed on the latest updates from the partnership.
